When people ask me “what does necrotic skin tissue smell like?”, I tell them it’s not just an odor—it’s often the body’s earliest alarm before infection spreads. In my years around wound care, I’ve noticed the smell is unlike anything else: sharp, foul, sometimes sickly sweet. Patients and families who encounter it for the first time often describe it as unforgettable. For me, it has been a reliable early sign long before scans or lab work confirmed what was happening beneath the skin.
That is why odor matters. I’ve seen cases where recognizing the smell early allowed treatment teams to act before the infection advanced, and cases where ignoring it meant the infection spread dangerously through the body. This guide goes beyond definitions. Here, you’ll learn necrosis what does necrotic skin tissue smell like and when that odor means urgent care is the only safe choice.
Top Takeaways
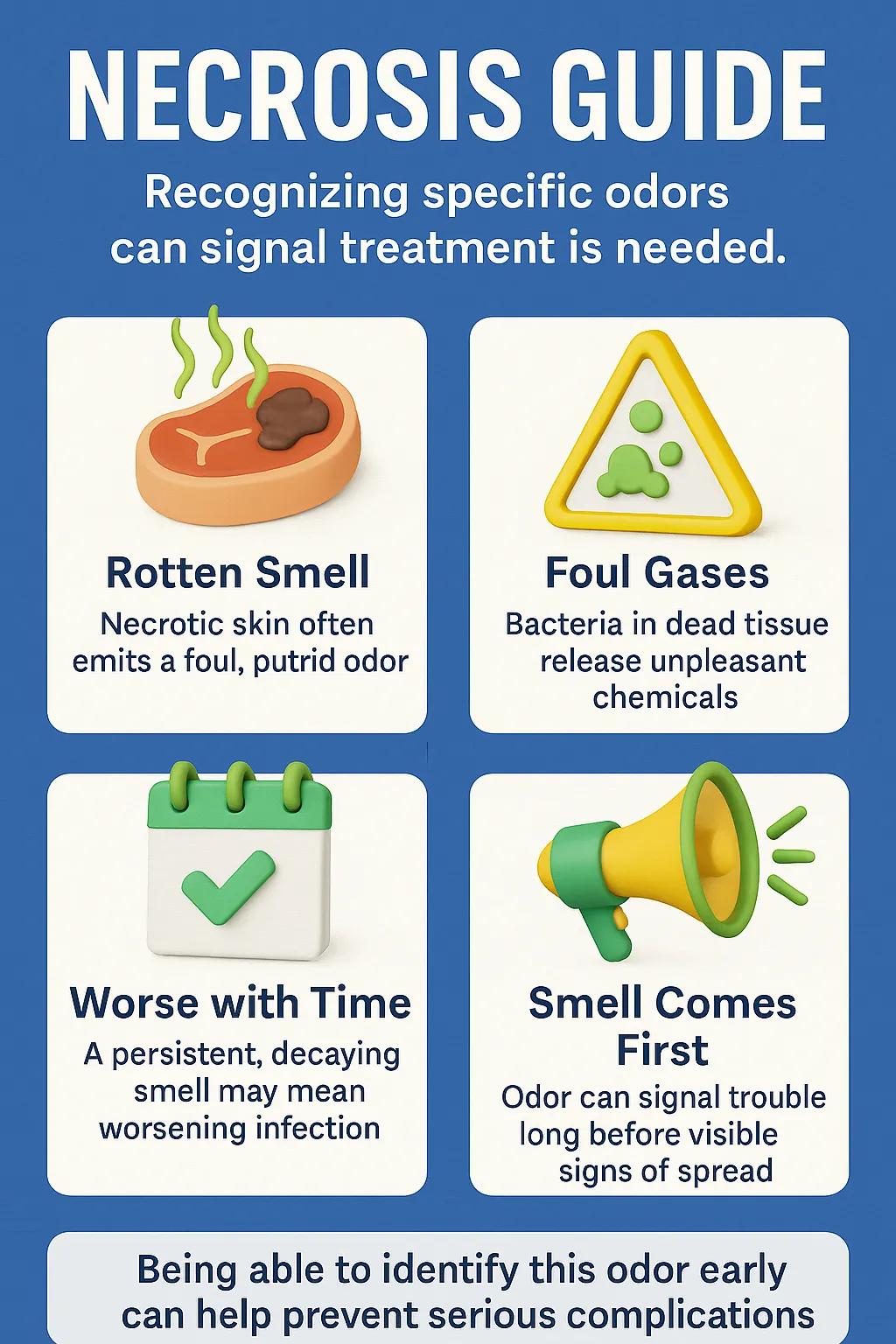
- Necrosis has a smell.Foul, putrid, or sweetly rotten odor comes before skin changes.
- Odor is an early sign.Smell reveals tissue death or infection sooner than tests.
- Act fast.Early care prevents severe complications and amputations.
- Trust your senses.Unusual wound odors should never be ignored.
- High-risk groups need checks.Diabetes, poor circulation, or immobility raise the risk.
Why Odor Appears Before Infection Spreads
Necrosis happens when skin tissue dies, usually because of poor blood flow, severe injury, or infection. One of the first and most telling signs is odor. People searching “what does necrotic skin tissue smell like” are often surprised to learn that the smell appears early, even before infection spreads widely through the body.
The odor is distinct—foul, putrid, sometimes sweetly rotten. It develops as bacteria break down dead cells and release gases and chemical compounds. In my experience, this odor often appears long before the skin turns black, hardens, or shows other visible changes. That’s why it’s considered a red flag: the body is warning you of hidden tissue death and possible infection under the surface.
Recognizing this smell matters because it offers a critical window of time. Acting quickly at this stage—seeking urgent medical care—can stop infection from spreading, promote faster wound healing, prevent serious complications, and sometimes save both life and limb.
“In my experience, the odor of necrotic skin tissue is one of the earliest and most reliable warning signs. Long before the skin turns black or hardened, that sharp, foul smell tells us infection and tissue death are already underway. Acting quickly at this stage can mean the difference between a simple treatment and a life-threatening complication.”
Case Study & Real-World Examples: Odor as the First Signal
Diabetic Foot Ulcer
Patient arrived with a “small sore.”
Looked mild: no black skin, no swelling.
Bandage removal revealed a sharp, foul, sickly sweet odor.
Tests confirmed hidden necrosis beneath healthy-looking skin.
Acting on smell led to fast treatment and saved the foot.
Bedsores in Elderly Patients
Pressure sores sometimes appear harmless on the surface.
Sudden putrid odor signals tissue death underneath.
Families often ask why smell matters if the wound looks fine.
In my experience, acting on odor early prevents severe infection.
Ignoring it often leads to dangerous, life-threatening outcomes.
Research Perspective
Advances in Skin & Wound Care identifies odor as a consistent marker of necrosis.
My experience confirms this: odor often appears before test results.
The nose gives one of the earliest and most honest warnings.
Patient arrived with a “small sore.”
Looked mild: no black skin, no swelling.
Bandage removal revealed a sharp, foul, sickly sweet odor.
Tests confirmed hidden necrosis beneath healthy-looking skin.
Acting on smell led to fast treatment and saved the foot.
Pressure sores sometimes appear harmless on the surface.
Sudden putrid odor signals tissue death underneath.
Families often ask why smell matters if the wound looks fine.
In my experience, acting on odor early prevents severe infection.
Ignoring it often leads to dangerous, life-threatening outcomes.
Advances in Skin & Wound Care identifies odor as a consistent marker of necrosis.
My experience confirms this: odor often appears before test results.
The nose gives one of the earliest and most honest warnings.
Supporting Statistics & Insights
Pressure ulcers
2.5 million+ cases in the U.S. each year (AHRQ).
High risk of infection and tissue death.
In my experience, odor is often the first clue they’ve worsened.
Diabetic foot ulcers
19–34% lifetime risk for people with diabetes (Diabetes Journals).
Odor frequently signals worsening before visible skin changes.
Annual U.S. cases
1.6 million diabetic foot ulcers each year; 50–60% become infected (JAMA).
In practice, infection plus odor often points to necrosis.
Pressure ulcers
2.5 million+ cases in the U.S. each year (AHRQ).
High risk of infection and tissue death.
In my experience, odor is often the first clue they’ve worsened.
Diabetic foot ulcers
19–34% lifetime risk for people with diabetes (Diabetes Journals).
Odor frequently signals worsening before visible skin changes.
Annual U.S. cases
1.6 million diabetic foot ulcers each year; 50–60% become infected (JAMA).
In practice, infection plus odor often points to necrosis.
Final Thought & Opinion
Necrosis is real.
The smell is more than unpleasant—it’s the body’s alarm for tissue death and infection.
Odor often appears first.
I’ve seen wounds that looked mild but smelled sharp and foul.
The odor revealed hidden necrosis before the skin changed.
Acting on smell saved patients from amputations.
Ignoring it led to worse outcomes.
My perspective.
Odor should be treated like pain, swelling, or fever.
It is one of the body’s earliest and most reliable warning systems.
Scans and lab tests are vital, but smell remains a powerful diagnostic tool.
Teaching families and caregivers to trust their senses could save lives.
Necrosis is real.
The smell is more than unpleasant—it’s the body’s alarm for tissue death and infection.
Odor often appears first.
I’ve seen wounds that looked mild but smelled sharp and foul.
The odor revealed hidden necrosis before the skin changed.
Acting on smell saved patients from amputations.
Ignoring it led to worse outcomes.
My perspective.
Odor should be treated like pain, swelling, or fever.
It is one of the body’s earliest and most reliable warning systems.
Scans and lab tests are vital, but smell remains a powerful diagnostic tool.
Teaching families and caregivers to trust their senses could save lives.
Next Steps
Seek urgent care.
Call your doctor, wound-care specialist, or go to urgent care.
Document details.
Note when the odor started, how it smells, and any wound changes.
Avoid home remedies.
Don’t scrape, cut, or mask the odor with creams or powders.
Watch for warning signs.
Fever, swelling, redness, or pain may signal infection.
Involve others.
Teach caregivers or family to recognize necrotic odor early.
Stay proactive.
At-risk groups—diabetes, poor circulation, immobility—need regular wound checks.
Proper wound management is essential—by seeking urgent care, documenting changes, avoiding risky home remedies, and staying proactive, you can catch problems early and prevent serious infections.
Seek urgent care.
Call your doctor, wound-care specialist, or go to urgent care.
Document details.
Note when the odor started, how it smells, and any wound changes.
Avoid home remedies.
Don’t scrape, cut, or mask the odor with creams or powders.
Watch for warning signs.
Fever, swelling, redness, or pain may signal infection.
Involve others.
Teach caregivers or family to recognize necrotic odor early.
Stay proactive.
At-risk groups—diabetes, poor circulation, immobility—need regular wound checks.